Welcome to the first in a series of Self-Help Guidelines for Managing your Own Injuries – whether at home or at work. Â Obviously this isn’t a replacement for seeking help from a Qualified Physiotherapist should you need it, but often you can limit damage by assisting yourself in the first instance following an injury.
For our first instalment we will be looking at two common complaints, Tennis Elbow and Frozen Shoulder.
Managing Tennis Elbow
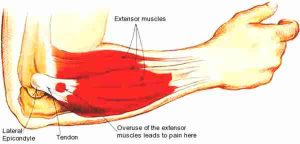 Tennis elbow (also known as lateral epicondylitis) is characterised by pain in the Extensor muscle/tendon, located on the outer side of the elbow joint. PAIN can be felt in the middle of the forearm (the muscle belly) all the way up to the bony part of the outer elbow joint (the tendon insertion). It usually results from an OVERUSE injury, whereby repetitive movements take their toll on a relatively small muscle and/or tendon. Fewer cases occur due to direct impact or injuries.
Tennis elbow (also known as lateral epicondylitis) is characterised by pain in the Extensor muscle/tendon, located on the outer side of the elbow joint. PAIN can be felt in the middle of the forearm (the muscle belly) all the way up to the bony part of the outer elbow joint (the tendon insertion). It usually results from an OVERUSE injury, whereby repetitive movements take their toll on a relatively small muscle and/or tendon. Fewer cases occur due to direct impact or injuries.
What causes tennis elbow?
As mentioned, repetitive overuse is usually to blame , but you’ve don’t have to be a tennis player to pick up this injury (although research indicates up to 45% of daily tennis players and 20% of twice weekly players will suffer with this at some point). Evidence further states that the usual incidence occurs between 40-50 years of age, although ultimately any age can be affected. Tennis elbow usually follows a bout of the Extensor muscles working harder than they are used to. There are a number of Extensor muscles that allow for the fingers and wrist to extend and they all originate via one tendon called the ‘Common Extensor Tendon’. The following are just some examples of how this happens:
- Poor keyboard/mouse set-up, e.g. a continually extended and rotated forearm
- Continuous gripping activities, e.g. DIY, manual labour
- Overuse using gardening equipment, e.g. shears
- Gripping and rotation activities, e.g. using a screwdriver to put up that flat-pack furniture, knitting, sewing
- Poor technique, e.g. faulty backhand during racket sports
- A different condition albeit less common condition known as Golfer’s elbow (also known as medial epicondylitis) affects the muscles and tendons on the inside of the elbow. This affects the opposite muscles of the forearm to the Extensors called the Flexor muscles/tendons. Golfer’s elbow can also arise from the above overuse activities.
Tennis Elbow Signs and Symptoms
- Pain over the outside of the elbow joint, or along the muscles on the outside of the forearm
- Weakness in the wrist that causes difficulty with normal tasks, e.g. lifting a plate or cup, opening doors, wringing a wet cloth, etc.
- Rarely swollen/inflamed due to the poor blood supply of the tendon
How is it treated?
 Tennis elbow is commonly known as a self-limiting condition, i.e. it can resolve completely on its own without intervention. However treatment depends on the amount of time since the initial onset of injury occurred – and there is no single treatment that has been shown to be completely effective at reducing this problem.
Tennis elbow is commonly known as a self-limiting condition, i.e. it can resolve completely on its own without intervention. However treatment depends on the amount of time since the initial onset of injury occurred – and there is no single treatment that has been shown to be completely effective at reducing this problem.
If this is a new/acute injury, pain can be reduced following the PRICE protocol. Resting from the aggravating activity is paramount in settling down any further symptoms. Anti-inflammatory medication can also be considered under the direction of your GP.
Physiotherapy Management of Tennis Elbow
As this acute phase settles, physiotherapy then starts to play an important role in recovery. Soft tissue massage and loosening any tight muscles/tendons is effective, along with appropriate stretching and strengthening of the Extensor muscles and tendons. It is important to stretch and strengthen the Extensor muscles and tendons in the correct manner; this is usually achieved by eccentric exercise – talk to your physiotherapist about these. Evidence shows this type of exercise to be one of the most effective strategies in settling down a tennis elbow.
Returning to work and offloading the tendon with a tennis elbow support/clasp is also useful as it can be difficult to change workplace techniques that require prolonged use of the hands/wrists. Talk with your employer with regards to a workstation assessment to ensure you are set-up correctly – whether this be desk based, on the factory floor or in the workshop.
For those who partake in racket sports, addressing technique and equipment is important; an incorrect grip is sometimes at fault, along with a racket that is too heavy or too light even. Increasing the circumference of your grip can be helpful to prevent recurrence of a tennis elbow.
Long Term Management?
Occasionally, the above treatment options just aren’t enough to settle down a tennis elbow, especially if this has been a chronic problem. Shockwave therapy and injections of corticosteroids can be used and as a last resort and surgery may be considered to provide overall relief whilst managing injuries. These options are usually only considered once the conservative treatment options above have been exhausted or failed.
Self Help Treatment for Frozen Shoulder
 Also known as Adhesive Capsulitis, a frozen shoulder is a common shoulder condition that affects between 2-5% of the population, usually in people aged between 40 and 65 years and more usually women than men. It is characterised by an onset of pain and progressive stiffness that then takes over within the shoulder joint – classically neither you or anyone else (i.e. a physiotherapist or doctor) can move the shoulder joint. It affects everyone differently, ranging from only mild limitations of movements, to having barely any movement at all in the shoulder.
Also known as Adhesive Capsulitis, a frozen shoulder is a common shoulder condition that affects between 2-5% of the population, usually in people aged between 40 and 65 years and more usually women than men. It is characterised by an onset of pain and progressive stiffness that then takes over within the shoulder joint – classically neither you or anyone else (i.e. a physiotherapist or doctor) can move the shoulder joint. It affects everyone differently, ranging from only mild limitations of movements, to having barely any movement at all in the shoulder.
It should be noted that a frozen shoulder is not a form of arthritis and does not affect other joints within the body.
What are adhesive capsulitis causes?
The glenohumeral (shoulder) joint is surrounded by a thin capsule that surrounds the joint. Its responsibility is to house synovial fluid, a lubricating fluid that keeps the joint supple. A frozen shoulder occurs when this joint capsule becomes inflamed and then thickens and gets ‘sticky’ – it then tightens as scar tissue and adhesions can sometimes builds up within the capsule. There is no known cause as to exactly why this happens; it can come on inexplicably for no apparent reason. However, there are a few instances in literature whereby the incidence of a frozen shoulder is heightened:
- Recent cardiac/heart surgery
- Diabetes
- Trauma or falls onto the shoulder
- Prolonged immobility of the shoulder
The Main Frozen Shoulder Symptoms:
- Pain and/or stiffness in the shoulder
- Progressive loss of movement in the shoulder
- Sleeping on the affected shoulder, although sometimes even sleeping on the other side can be painful too
- Difficulty with certain movements, e.g. washing your hair, reaching behind your back, putting on a jacket, doing up a bra.
There are 3 phases to a frozen shoulder, whereby different symptoms are apparent:
- FREEZING STAGE – Pain is at most obvious and limits the ability to move the shoulder joint. Usually lasts 2-9 months.
- FROZEN STAGE – Pain begins to reduce and stiffness is the main problem that limits movement. Wasting of the shoulder muscles may begin due to less usage of the shoulder. Usually lasts 4-12 months.
- THAWING STAGE – stiffness/pain gradually improves. Usually lasts 5 months-years.
Diagnosis is made following a clinical assessment from your GP or physiotherapist. Classically, the shoulder joint is tested in different ways to try and achieve full, normal movement; if this cannot be achieved actively (you performing certain movements) or passively (someone else moving the shoulder for you), then a frozen shoulder can be suspected. The strength of muscles is usually good, although pain can sometimes inhibit and mask weak muscles. Confirmation via scans is not usually required and x-rays are only used to rule out any other shoulder problems, e.g. arthritis.
How Frozen Shoulder Is Treated
Unfortunately, there is no cure for a frozen shoulder, it has to run its course and as seen above, this can vary over months-years. However, early treatment of a frozen shoulder is very important – the earlier that the pain can be treated and the earlier that movement can be salvaged, the quicker the recovery. Ultimately the aim of treatment is to control pain and maintain as much functional movement within the shoulder joint as possible.
In the early phases, i.e. the FREEZING phase, adequate pain control is imperative. This can be achieved with analgesia and anti-inflammatory medication – talk to your GP about these. Hot/cold therapy can be used over the painful shoulder via hot water bottles or ice packs wrapped in pillow cases/tea towels; try alternating 10 minutes of each when particularly painful. TENs machines can also be used on a daily basis to try and calm the pain down, albeit the evidence behind these varies greatly. Acupuncture can also potentially be utilised to control pain. Exercise can start in the form of pendular exercises – a way of ensuring gentle movement/mobilisation of the shoulder joint is maintained whilst trying not to cause to much pain. Active assisted movements utilise sticks and brooms around the home to ensure that movement is maintained in varying planes of movement.
As the frozen shoulder progresses from the FREEZING-FROZEN phase, more movement is required as pain allows. Active assisted exercises can be progressed and capsular stretches can start, again within pain-free limitations.
Physiotherapy and Frozen Shoulder Syndrome
Throughout a frozen shoulder, physiotherapy is warranted; this can involve supervised exercise prescription, capsular stretching, joint mobilisation, soft tissue massage or general advice about the management of a frozen shoulder. Sometimes however, if the pain is too great in the shoulder, injections may be required to allow for pain-free periods allowing more mobility exercises to be achieved.
Surgery is uncommon with frozen shoulders, although if conservative treatment fails it can be considered. Manipulation Under Anaesthetic (MUA) of the shoulder joint is one possible route, whilst an arthroscopic (keyhole) capsular release can also be used. With both surgeries, physiotherapy is required in the form of the above. Symptoms can however sometimes even persist after these surgical interventions.
Do you have on-going issues with Tennis Elbow or Frozen Shoulder? Â If so we can help.
Visit our Contact Us page to book or call 01582 761448.
acute soft tissue management, frozen shoulder, sports injuries, tennis elbow,



